Explore Menstruation Matters archive
ANNOUNCEMENT: Menstruation Matters, the blog of the Society for Menstrual Cycle Research, is taking a break from regular posting. However, the archive remains available to researchers, educators, advocates, and anyone else interested in the menstrual cycle....

Menstrual Health Hub connects community
Influencing, connecting & uniting the menstrual health community Guest Post by Danielle Keiser and Milena Bacalja Perianes: The menstrual health community is growing exponentially. A multitude of organizations, researchers, companies, and advocates taking up the...

Congresswoman Carolyn B. Maloney receives Making Menstruation Award
Congresswoman Carolyn B. Maloney is the third recipient of the Making Menstruation Matter Award in recognition for her tireless advocacy of federal legislation on behalf of women's reproductive health, especially her sponsorship of the Robin Danielson Feminine Hygiene...

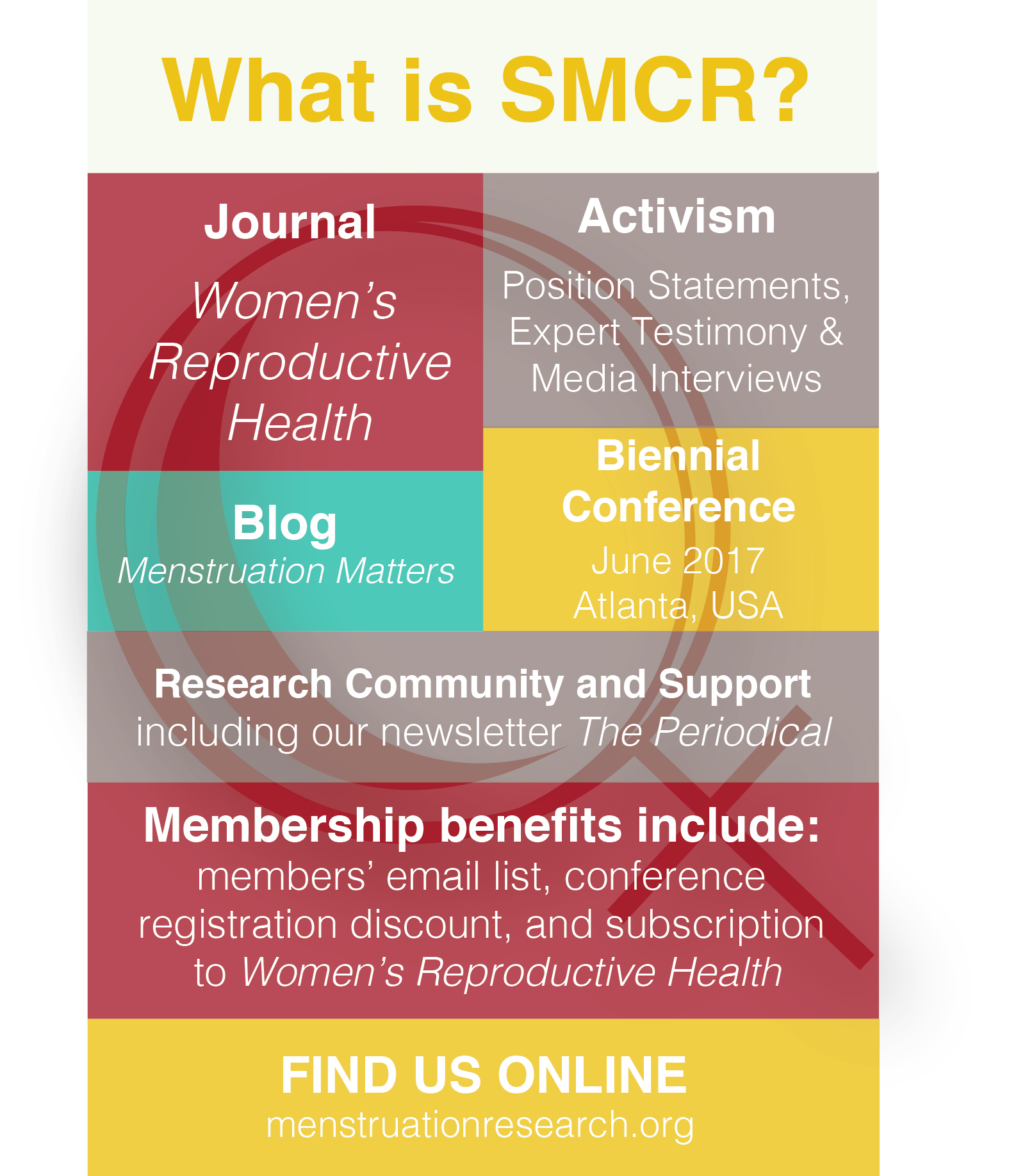
SMCR marks 40th anniversary in Atlanta
Convening at Kennesaw State University outside of Atlanta, Georgia, the Society for Menstrual Cycle Research celebrated its 40th Anniversary June 22-24, 2017. The traditional symbol for a 40th tribute is the ruby gemstone, an apt image for an organization dedicated to...
TV series “I Love Dick” takes on menstruation
"I Love Dick," the provocatively titled new Amazon video series that premiered recently to considerable fanfare, joins the still small canon of films and TV programs taking on the topic of how sexual and social relationships are shaped by the presence of...

DC Rally May 23 for Safe Feminine Care Products
Guest Post by Sarada Tangirala When Ignorance Isn’t Bliss: Rally in Washington for Safe Feminine Care Products Women’s Voices for the Earth (WVE) is hosting a rally at the nation’s capital to raise awareness of the need for safe feminine care products. Representative...

